The Service Design Award is currently open for submission again. Submit your project for a chance to win and present at the Service Design Global Conference in Toronto this year.
Introduction
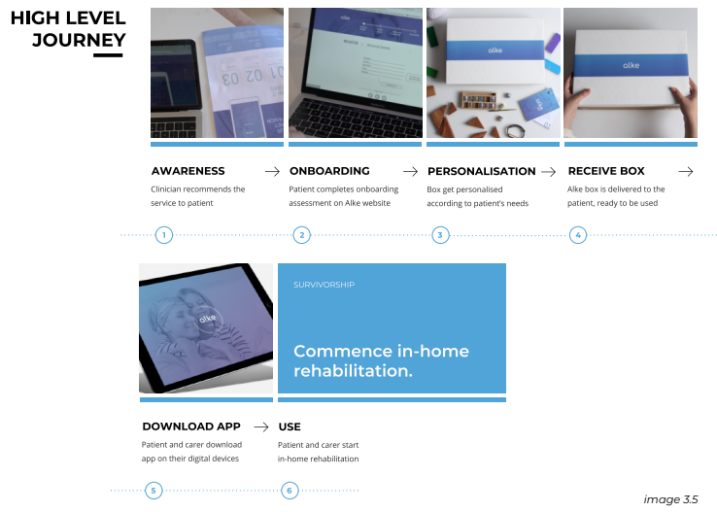
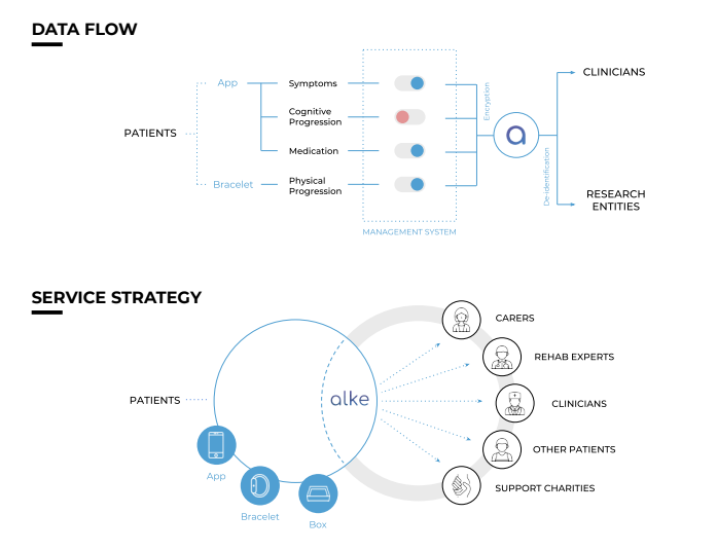
In the UK, there are more than 11,500 new cases of a brain tumours every year, which is equal to a 34% increase in the incidence rate of brain tumour since the 90s. At least 102,000 children and adults are currently living with a brain tumour in the UK alone. This report introduces Alke, a service for people with a brain tumours and their carers, that helps them understand, adapt and easily manage their rehabilitation on a daily basis. Alke has the potential of facilitating the rehabilitation experience of patients with a brain tumour and their carers by enhancing self- management, introducing a digital communication channel for patients and their carers to connect with clinicians, while providing a holistic and personalised approach that understands the patient’s status and supports them in strengthening their cognitive and physical functions through engaging activities. The overall aim of the service is to enable patients to be in charge of their rehabilitation journey. With Alke, we are more than just creating a new healthcare service. We aim to spread the awareness for brain tumour and interconnect patients, carers, physicians, and the support communities. The project has been validated by users, experts in healthcare and technology but has not been implemented.
Process
The process methodology that we used was the Design Council’s double diamond, with great focus on having a user-centric empathetic approach. Using this approach meant that no assumptions were made at the start about the nature of the problems and we based all our insights on the exact needs and challenges that were communicated to us from the users, the people with a brain tumour and their carers. We sought to develop an inclusive and empowering way of creating change to improve the lives of all those involved. In overview, our design process followed 4 stages: Discovery, Define, Develop and Deliver & Validation.
DISCOVERY
The purpose of this stage was to understand the current system, as well as engage with the primary stakeholders to understand their pains. To begin our research into understanding our stakeholders, we conducted numerous interviews, travelling around UK (London, Basildon, Birmingham, Worcester, Walsall, Derby) in order to meet with patients, carers, and clinicians. As a result, we met with 3 clinicians, 4 patients including 1 terminal patient, 6 carers, as well as the Head of Support of a Brain Tumour Support Charity.
For this stage, we used exploration activities, such as journey mapping (image 1.1) as our primary tool. We wanted to listen and experience the whole journey from the patients’ and the carers’ perspective and highlight, not only the functional bits of the process but also their emotional rollercoasters. This helped us tremendously in understanding the timeframe of battling the tumour, but also what their life was like before the tumour, and how it has changed after the tumour. Most importantly we learned about how they were coping with their current issues and the system and the techniques they had to develop themselves in order to overcome the challenges. For example, one of the carers whose late wife has had difficulty with mobility and suffered from expressive aphasia (difficulty finding the words to express their thoughts), had to develop a technique himself in order to better communicate with her. They had their own system, where his wife would bang her stick twice on the floor if she wanted him to come upstairs. In another example, a patient noticed that often times, the 10-minute consultations were short, rushed, and overwhelmed him with information about which he had no time to look back and ask
questions. So he started a diary, taking notes about his symptoms, doubts, curiosities, and emotions whenever he felt like it was important, in order to share them with the consultants. These insights became very valuable to us in creating touch points and service principles.
Along with primary sources, we followed blogs and read books written by patients themselves, survivors and carers, and generated journey maps for those experiences as well. We were able to learn the pains and emotions, and more accurately document all steps of the experience. In addition to the activity based interviews with the main stakeholders, we created an online survey and shared it on various social media support groups for brain tumour patients and carers. We received a total of 42 responses, 29 from patients and 13 carers. The survey gave us a wide-ranging understanding, in a quantitative manner, of the issues they are facing and verified the insights we had already obtained through the in-depth interviews.











Share your thoughts
0 RepliesPlease login to comment